There are more and more studies raising alarms about the impact of being lonely on our health. And the conclusions of those studies really shocked me so I decided to summarize and share this research in this blog. But first of all, how did they define loneliness? Loneliness is the cognitive discomfort or uneasiness of […]
3049 Kingston Road, Scarborough ON M1M 1P1
Opening Hours : Monday to Friday - 9:00am to 6:00pm
Contact : 416.261.8181
All Posts in Category: Mental Health
Ashwagandha
“Ashwagandha” is a medicinal herb commonly used in traditional Ayurvedic medicine, which originated in India. Its botanical name is Withania somnifera, and it is also known as Indian ginseng or winter cherry. Ashwagandha has also been called the king of Ayurvedic herbs and has been used in India for nearly 5,000 years. The name of […]
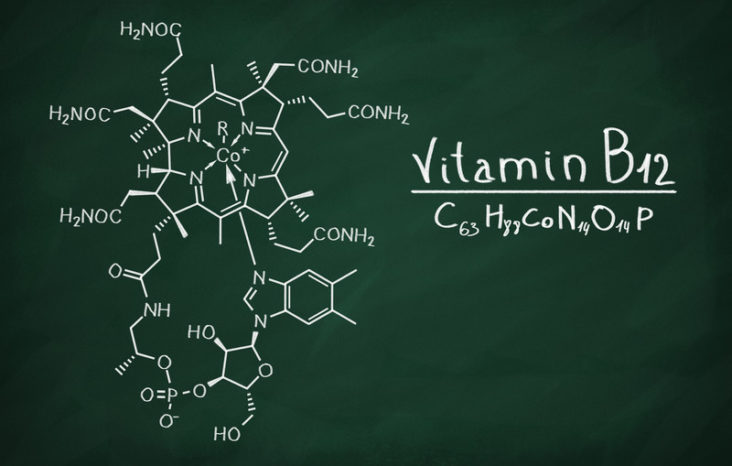
Vitamin B12
Vitamin B12 (cobalamin) is a water-soluble vitamin that plays essential roles in red blood cell formation, cell/energy metabolism, nervous system function and the production of DNA. Vitamin B12 is an elaborate molecular jigsaw involving around 30 individual components. It is unique among the vitamins in that it is only made by certain bacteria, but the […]

AUTISM
The first appearance of autism in historical literature was in 1911 by Eugen Bleuler, a psychiatrist from Switzerland, who used the term to describe a unique cluster of symptoms that were traditionally thought to simply be symptoms of schizophrenia (Bleuler also coined the terms schizophrenia and schizoid and was a contemporary of Freud; his students […]

Cannabis: the good and the bad
Here is a summary of the positive effects of cannabis and the adverse effects that it can exert on humans: The bad: Long-term use of either cannabis or cannabis-based drugs impairs memory and learning, say researchers. Their study has implications for both recreational users and people who use the drug to combat epilepsy, multiple sclerosis […]

Psychedelics
Psychedelics are powerful psychoactive substances that alter perception and mood and affect numerous cognitive processes. They can cause thought and visual/auditory changes and induce an altered state of consciousness. They are generally considered physiologically safe and do not lead to dependence or addiction. Initially these molecules were called hallucinogens. But the researchers soon discover that […]

Exercise and its benefits
We all know (hopefully!) that exercise is important in our daily lives, but we may not know why or what are the benefits of exercise. I would like to emphasize from the beginning that these benefits are backed up by rigorous research and science and are truly amazing. Before I present these benefits, it’s important […]

Stress vs Depression
Some stress, caused by regular life challenges, is unavoidable. And while feeling nervous about a date, a work presentation or frustrated by an overprotecting parent or an obnoxious boss is not fun, nobody would compare it to the challenge that is depression, a serious illness. Severe stress, however, is a different story. As anyone who […]

Catatonia
Catatonia is a fascinating medical condition marked by changes in muscle tone or activity associated with a large number of serious mental and physical illnesses. It was described for the first time by a German psychiatrist, Karl Ludwig Kahlbaum in 1874. The exact mechanisms underlying the pathophysiology of catatonia still remain a mystery. It seems […]
