Screening in medicine means checking for a disease in a group of people who don’t present any symptoms of the disease. Screening tests help doctors find breast cancer before any symptoms develop. When breast cancer is found and treated early, the chances of successful treatment are better (better outcome).
But before discussing the screening guidelines in Canada, let’s take a look at some statistics for Breast Cancer in Canada. These are numbers from Canadian Cancer Society.
Breast cancer is the most common cancer among Canadian women (excluding non-melanoma skin cancers). It is the 2nd leading cause of death from cancer in Canadian women. Breast cancer can also occur in men, but it is not common.

Incidence and mortality
Incidence is the number of new cases of cancer. Mortality is the number of deaths due to cancer. The following incidence and mortality statistics are estimated using the most up-to-date actual data available.
In 2017, an estimated:
- 26,300 women were diagnosed with breast cancer. This represents 25% of all new cancer cases in women in 2017.
- 5,000 women died from breast cancer. This represents 13% of all cancer deaths in women in 2017.
- On average, 72 Canadian women were diagnosed with breast cancer every day.
- On average, 14 Canadian women died from breast cancer every day.
- It is estimated that about 1 in 8 Canadian women will develop breast cancer during her lifetime and 1 in 31 will die from it.
- 230 men were diagnosed with breast cancer and 60 died from breast cancer.
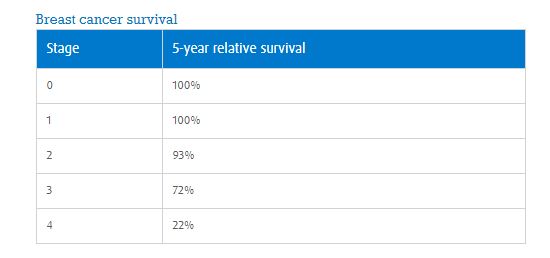
Survival – the most common used statistics are those by stage.
And now, let’s get back to screening.
Canadian Task Force on Preventative Health Care (CTFPH), an independent body of 15 primary care and prevention experts, was established by the Public Health Agency of Canada (PHAC) to develop clinical practice guidelines that support primary care providers in delivering preventive health care.
This Task Force published in 2011 the following guidelines:
- For women aged 40–49 we recommend not routinely screening with mammography. Women in this age group face a higher risk of potential harms from false positives, overdiagnosis and overtreatment compared with other age groups, and the absolute benefit is smaller.
(Weak recommendation; moderate quality evidence)
- For women aged 50–69 years we recommend routinely screening with mammography every 2 to 3 years.
(Weak recommendation; moderate quality evidence)
- For women aged 70–74 we recommend routinely screening with mammography every 2 to 3 years.
(Weak recommendation; low quality evidence)

These recommendations do not apply to women at higher risk due to personal history of breast cancer, history of breast cancer in first degree relative, known BRCA1/BRCA2 mutation, or women who had chest radiation therapy before 30 years of age or within the past eight years.
The Task Force issued another recommendation these days, for women aged 40-49, that emphasized shared decision-making in a potential screening and the conditional aspect on the relative value a woman places on possible benefits and harms of screening. (Simply put it: if a woman 40-49 yo wants a screening with mammography,the doctor must inform her of risks and benefits and do it.)
Before I wrap it up, please also be aware that:
- It is always your personal decision to be screened for breast cancer. Sometimes women forget this.
- The guidelines are for screening tests and not for diagnostic tests. What’s the difference?
The primary purpose of screening tests is to detect early disease or risk factors for disease in large numbers of apparently healthy individuals.
The purpose of a diagnostic test is to establish the presence (or absence) of disease as a basis for treatment decisions in symptomatic or screen positive individuals (confirmatory test). The gold standard for diagnosing breast cancer is a Needle Biopsy, not a mammograph.
- No breast screening test is 100% accurate and a screening test may show cancer when it isn’t actually there, or it may miss cancer that is present.
- Screening Guidelines are for women of average risk. If you are at higher risk due to family history or another factor, you may need to be screened more often than the recommended guidelines. Consult a doctor to determine your personal risk.
- It is important to become familiar with how your breasts look and feel so you can easily notice any changes. Report any breast changes promptly to your doctor.
- According to the Task Force, an emerging risk factor not yet used to place women in the high-risk group is the degree of breast density. Breast density may impact screening accuracy and is becoming a well-recognized, and significant risk factor for breast cancer.Women with dense breasts have 3 to 5 times greater lifetime risk of developing breast cancer than women with mostly fatty breasts, regardless of other risk factors (McCormack & dosSantos Silva, 2006; Boyd et al., 2007). If you are unsure about your breast density, it is important to speak to your doctor.
Here at the Family Naturopathic Clinic, we offer another screening technique for cancer – THERMOGRAPHY.
Thermography uses a heat-sensitive infrared camera to take images of the body and detect blood flow patterns.
Studies have shown that thermography can detect early danger signs in the body years before other tools, and it has been shown to be effective in finding early signs of breast disease up to 5 years before mammography may detect it.
